
- Flawless
- Botanicals
We are botanical explorers
Botalys is a supplier of premium ingredients for the Nutraceutical and Cosmeceutical industries.
We make the impossible sourcing of rare botanicals possible and sustainable, allowing our clients to harness the full potential of biodiversity while preserving it.
Start your Journey
Restoring the Thrill for Botanical Exploration
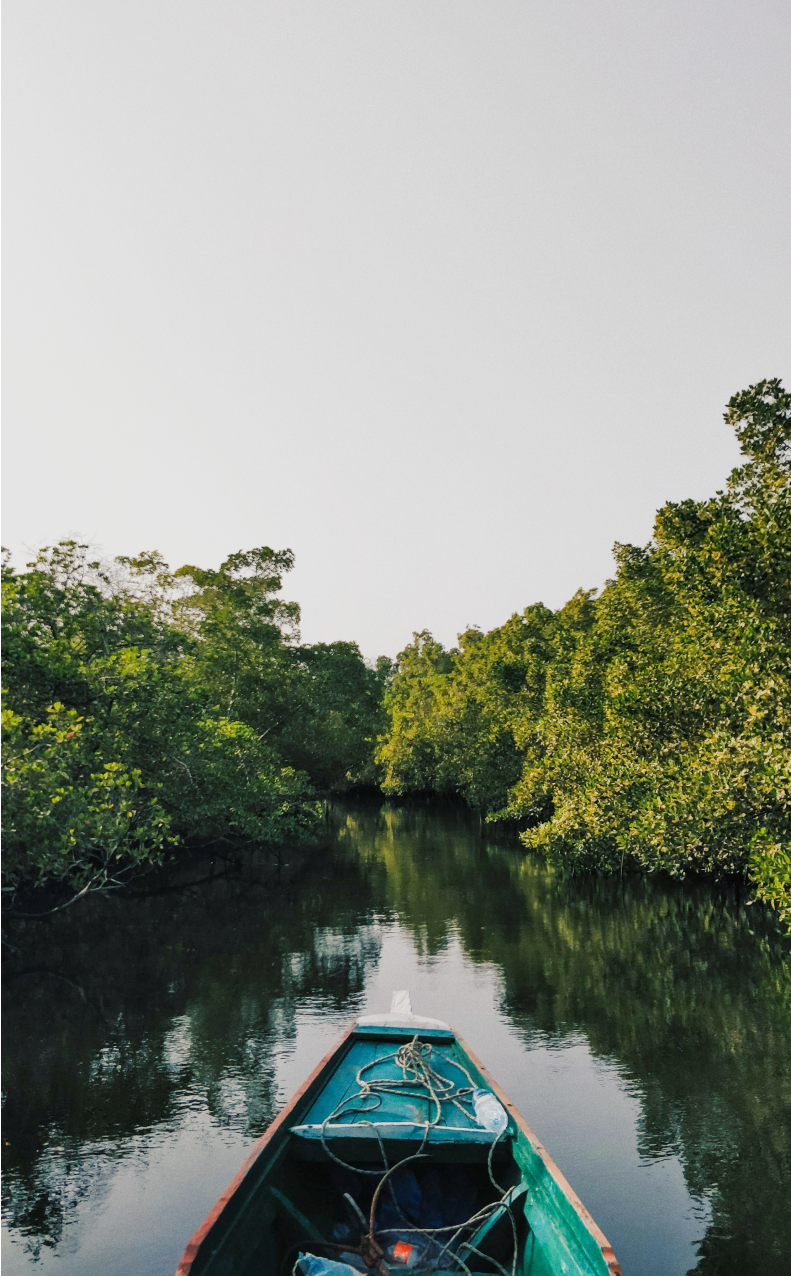
Venture off-trail
Biomimetic Farming Technology is a unique opportunity for you to explore uncharted botanical territories.

Upgrade your standards
BOTALYS is committed to providing meticulous brands like yours the uncompromising quality botanicals they deserve.

Protect wild biotopes
BOTALYS grows the most pristine botanicals in the world without plundering wild biotopes, ushering in a new era of truly sustainable phytoactive ingredients.

Let's go further together
Looking to harness the power of rare medicinal plants or explore the innovations of Biomimetic Indoor Farming? Curious about synergizing phytonutrients with emerging trends for unique Nutraceutical formulas? Let's turn your vision into reality. We're here to help.
Contact us